Simplify Healthcare Hurdles!
Technology | Process | Collaboration
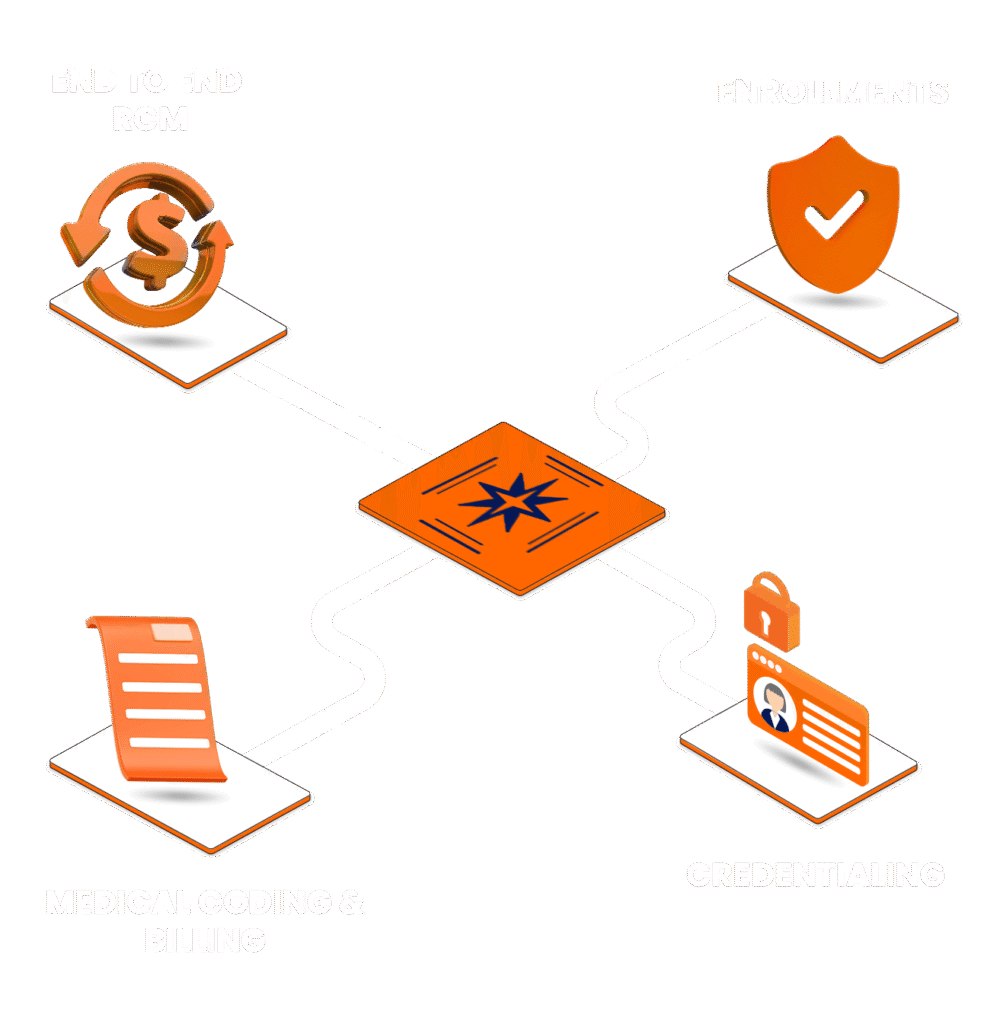
Why Choose Vanaa?
- Customizable Revenue Cycle Management Modules
- Faster Credentialing & Enrollment
- Faster Approvals & Claims Settelment
- Trsuted By Industry Leaders
Professional Healthcare Management Solutions
Credentialing and Enrollment
Streamline your provider onboarding with Vanaa’s Healthcare Credentialing and Enrollment Services. We ensure accurate documentation, faster payer approvals, and compliance driven processes to help you avoid delays, reduce denials, and accelerate reimbursements.
- Provider Credentialing
- Payer Enrollment
- CAQH Management
- Documentation Support
- Re-Credentialing & Renewals
Revenue Cycle Management
Optimize your revenue cycle with Vanaa’s end to end RCM Services. From patient registration to final payment posting, we manage billing, coding, claims, and collections that helps you in reducing denials, improving cash flow, and maximizing reimbursements.
- Medical Coding & Billing
- Claims Submission & Scrubbing
- Denial Management
- Accounts Receivable (A/R) Management
- Compliance & Audit Support
Faster enrollments, Accurate verifications, Seamless compliance.
Time Savings
Vanaa’s automated healthcare solutions reduce manual effort and cut financial administrative workloads by up to 50%, helping providers save time, lower costs, and focus more on patient care.
Increase Profitability
Boost efficiency and achieve up to 20% higher profitability while maintaining compliance and patient satisfaction.
Over 4m+ provider credentialing and payer enrollments completed ensuring accuracy, compliance, and speed.
Risk Reduction
Mitigate compliance risks, minimize claim denials, and safeguard your revenue with our proactive, audit-ready healthcare solutions designed to keep your operations secure and reliable.
Your Time is Valuable.
We Simplify Healthcare Operations for You.
Onboarding Process
Step 1: No cost, no obligation consult.
We understand your practice needs, challenges, and revenue goals.
Step 2: Current state analysis with action plan
Gather all provider details, credentials, and payer information.
Step 3: Action plan with timelines to achieve the desired state
Configure RCM/credentialing workflows, compliance checks, and reporting tools.
Step 4: Internal prop. system set up and Account Management Executive assigned.
Ensure smooth operations, track performance, and provide ongoing assistance.
Nationwide
Payer Network Access
Medicare, Medicaid and Private Commercials plus LOBs including HMOs, PPOs etc.

Tailored Solutions For All Specialities
OBGYN
Urology
Radiology
Durable medical equipment
Chiropractic
Internal medicine
Laboratory
Sleep medicine
CMH
Physical therapy
Hospitals
Cardiology
Behavioral health
Orthopedic
Anesthesiology
Surgery
Physician group practices
Durable medical equipment
Customized 360 professional services designed to meet the unique needs of every medical specialty.
Compliance That Protects Your Practice

Trusted by Leading Healthcare Providers
Years of Experience
Satisfied Clients
Monthly Reimbursements
Provider Network
In Cost Savings
Includes savvy providers & our clients.
Mr. Sarang Patel
Mr. Taylor Henrick
Ms. Bridgette Trader
Partnering for Success, Loved for Results.













David Miller

Dr. Rebbeca Parker

Michael Thompson

Michael Roberts

Dr. Maria Sancez

Dr. Jason Miller

Dr. Emily Johnson

Ros Eckelberry
What Our Clients Say
Let’s Build Your Healthcare Success
Request a Consultation

No Cost No Obligation Consult
By submitting this form you agree to our Privacy Policy. Vanaa may contact you via email or phone for scheduling or marketing purposes.
Real Results. Real Impact.
General FAQ's
What services does Vanaa provide?
Vanaa delivers end-to-end Revenue Cycle Management (RCM), credentialing, payer enrollment, licensure, medical coding, billing, denial management, and revenue analytics. Our automation first workflows have helped practices cut denials by 22% and improve net collections by 18% within 6 months.
Who can benefit from Vanaa’s services?
We serve independent providers, multi-specialty hospitals, behavioral health and telehealth practices. For example, a 20-provider group practice improved claim turnaround time from 46 to 18 days after onboarding with us.
How does Vanaa ensure compliance and data security?
Our operations are fully HIPAA-compliant. We use role-based access, encryption at rest/in transit and AI-driven monitoring for anomalies. In the last 5 years of audits, we’ve had 0 HIPAA violations or data breaches across all client accounts.
What results can I expect with Vanaa?
Providers typically see:
- 15–20% higher reimbursements
- 25% reduction in AR days
- First-pass acceptance rates above 95%
These outcomes are benchmarked against payer data from our national client base.
Can Vanaa integrate with my current EHR or PMS?
Yes. We’ve integrated with leading systems like Epic, Athenahealth, Cerner, eClinicalWorks, and more. On average, integration takes 2–3 weeks, depending on your vendor and data migration readiness.
What makes Vanaa different from other RCM companies?
Most firms either offer staff augmentation or rigid automation. Vanaa blends both. With AI exception management and 10+ professional expertise, we don’t just process claims. We optimize them for payer-specific compliance, reducing resubmissions by 30%.
Vanaa:
Smarter Services, Powered by AI.
You can unsubscribe at any time using the link in the footer of our emails.