Provider Credentialing & Enrollment Services
Streamline your provider onboarding with Vanaa’s Credentialing & Enrollment Services. We ensure accurate documentation, faster payer approvals, and compliance driven processes to help you avoid delays, reduce denials, and accelerate reimbursements.
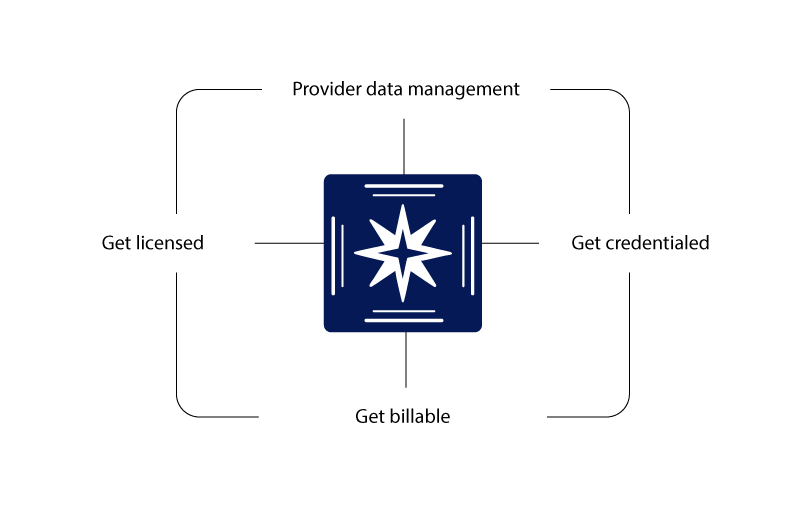
Credentialing & Enrollments Simplified
Managing provider credentialing and payer enrollment can be complex, time consuming, and error prone. Our Healthcare Credentialing and Enrollment Services ensure accurate documentation, faster approvals, and complete compliance, so your organization can focus on delivering quality patient care while we handle the backend.
- Provider Credentialing – Initial credentialing and re-credentialing with payers, hospitals, and networks.
- Payer Enrollment – Enroll with Medicare, Medicaid, and commercial insurers without delays.
- CAQH Management – Setup, maintenance, and ongoing attestation support.
- Documentation Support – Accurate preparation and submission of provider applications.
- Re-Credentialing & Renewals – Stay compliant with timely renewals and updates.
- Compliance & Audit Ready – Ensure adherence to payer and regulatory requirements.
- Status Tracking & Reporting – Get transparent updates throughout the credentialing process.

78%
less time spent on operational tasks.
50%
reduction in credentialing time.
10%
reduction in contracting
Faster Onboarding, Faster Revenue
We combine decades of credentialing expertise with cutting-edge automation to handle even the most complex cases without guesswork or templates.
Accelerated Reimbursements – Reduce revenue delays with faster payer approvals.
Error Free Submissions – Minimize rejections through accurate documentation.
Peace of Mind – We manage end-to-end credentialing while you focus on patients.
Dynamic workflows that adapt in real time
Tasks are auto-sequenced based on payer, state, provider type, and historical outcomes, so nothing slips through the cracks
Data extraction that thinks like your team
Our models extract and standardize data from licenses, forms, and PDFs with expert-level accuracy, no templates required.
Insights that power better decisions
Turn operational data into actionable dashboards, helping you optimize performance, spot blockers, and prove ROI.
Outcomes That Scale With Your Organization
Vanaa’s purpose-built automation accelerates provider readiness, reduces delays, and scales operations without additional headcount.
Get Providers Billable Fast
Cut Onboarding Time
Automate Tedious Tasks
FAQ's
What is provider credentialing and why does it matter?
Credentialing validates a provider’s qualifications, licenses, and affiliations with payers. Without it, claims are denied outright. In our experience, practices lose up to $50,000/month in potential revenue when credentialing is mishandled or delayed.
How long does credentialing take?
On average, payer approvals range between 30–90 days. Using our automation-first workflows, we’ve reduced delays by 40%, with some enrollments completed in as little as 28 days (Medicare included).
Does Vanaa handle payer enrollment?
Yes. We cover Medicare, Medicaid, commercial, and private payers. For one telehealth provider, we enrolled 120+ clinicians across 5 payers in under 60 days, cutting onboarding time by half.
Can Vanaa manage CAQH profiles?
Yes. We manage setup, attestation, and quarterly updates. Practices we support have seen a 98% CAQH approval accuracy rate compared to the industry average of 85%.
Does Vanaa manage provider licensure?
Yes. We handle renewals, expirations, and multi-state filings. Our licensure monitoring system has helped practices avoid 100% of missed deadlines in the last 3 years.
What happens if credentialing is delayed?
Each month of delay equals lost claims. For example, a behavioral health facility we onboarded was losing $72,000 monthly before we cleaned up their credentialing backlog. Within 90 days, they achieved full payer participation.
Do you support multi-state and re-credentialing?
Yes. We manage initial credentialing and renewals across multiple states. On average, multi-state enrollments take 20% longer — but with our workflows, we cut that gap significantly.
How do you ensure accuracy in submissions?
We use triple-layer checks: AI verification, document audits, and human QC. This has driven our error rate below 1.5%, versus the industry norm of 8–10%.
Driving Growth Through Strategic Clarity
Solutions for All Specialities
OBGYN
Urology
Radiology
Durable medical equipment
Chiropractic
Internal medicine
Laboratory
Sleep medicine
CMH
Physical therapy
Hospitals
Cardiology
Behavioral health
Orthopedic
Anesthesiology
Surgery
Physician group practices
Durable medical equipment
serving more than 100+ Specialities..
Why Healthcare Leaders Trust Vanaa













Michael Roberts

Dr. Maria Sancez

